Compounding is generally a practice in which a licensed pharmacist, a licensed physician, or, in the case of an outsourcing facility, a person under the supervision of a licensed pharmacist, combines, mixes, or alters ingredients of a drug to create a medication tailored to the needs of an individual patient. Compounding typically occurs in pharmacies, although it may also occur in other settings.
Compounding facilities, including pharmacies, can play an important role in serving patient needs, such as in cases when patients cannot use commercially available drug products for various reasons (e.g., doses for paediatric populations may not be commercially available).
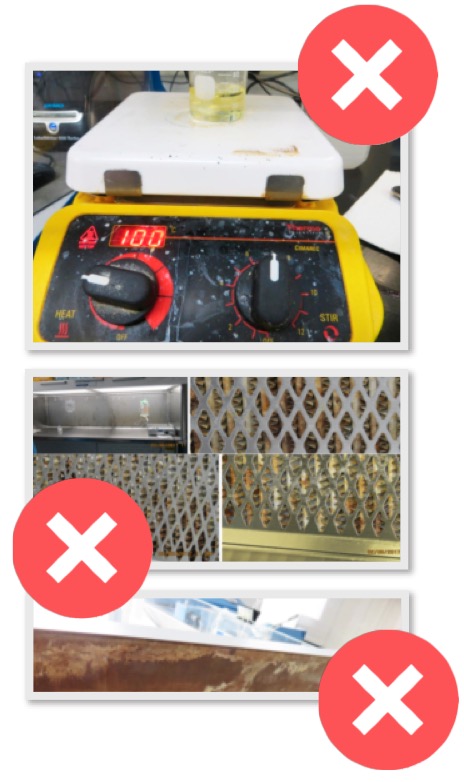
To protect patients, compounding facilities must meet federal and state standards that apply to them, including ensuring that compounded drugs are not prepared, packed, or held under insanitary conditions. Section 501(a)(2)(A) of the Federal Food, Drug, and Cosmetic Act (FD&C Act) states that a drug is deemed to be adulterated "if it has been prepared, packed, or held under insanitary conditions whereby it may have been contaminated with filth, or whereby it may have been rendered injurious to health."
During the 2012 fungal meningitis outbreak, contaminated steroid injections killed dozens
The FDA has investigated numerous adverse events, including deaths, caused by contaminated compounded drugs that were produced under insanitary conditions. During the 2012 fungal meningitis outbreak, contaminated steroid injections killed dozens and caused infections in more than 750 patients in numerous states. The FDA continues to observe insanitary conditions at compounding facilities that could cause drugs they prepare to become contaminated and produce a negative impact to patient health. Some compounding facilities have voluntarily recalled drugs and ceased compounding operations based on the FDA's observation of egregious insanitary conditions.
After years of inspecting compounding facilities, the FDA has identified patterns of insanitary conditions. In November 2020, the administration published a final guidance for industry on Insanitary Conditions at Compounding Facilities, which provides examples of insanitary conditions that the agency has commonly observed at compounding facilities.
Insanitary conditions
For compounders to understand how to prevent insanitary conditions, it is important to understand the different types of insanitary conditions commonly seen at compounding facilities, how these conditions arise, and how or why they can cause patient harm.
Insanitary conditions may result from, among other reasons:
- particulate matter such as dust, rust, glass, metal, hairs, fibres
- microbial contamination in or near the production areas
- chemical residues that may be sensitising, potent, hazardous, or are chemical impurities
- pests, including live or dead insects, rodents, or other animals that are in or near the production areas
Compounding cleanrooms are specifically designed to exclude or reduce the number of particles (microbial and non-microbial) and other sources that can lead to insanitary conditions.
Particulate matter and microbial contamination
Particulate matter can come from many sources. Dust particles are ubiquitous and surfaces in cleanrooms should routinely be cleaned. The floors, walls, and ceilings of cleanrooms should be made of smooth, hard surfaces that are easy to clean.

Improper construction materials (e.g., wood) may shed particles, be difficult to clean, and may also be damaged or further degraded by the harsh chemical disinfectants used in cleanrooms. Cardboard boxes also shed particles and are difficult to clean. Cleaning wipes and gowns made of shedding materials or gowns that are damaged or frayed could also be sources of particles.
Construction activities liberate microbial and non-microbial particles. Drug products should not be prepared in a facility while construction is ongoing without adequate controls to prevent contamination of the production area and the product.
Particles can also enter cleanrooms through air handling units (if the air is not properly filtered), from the space above the ceiling (if ceiling tiles are missing or misplaced), or from the space behind the walls via the air returns. Air should be supplied to the cleanrooms through appropriate air filters (e.g. HEPA filters) at sufficient velocity to sweep particles out of the cleanroom. The airflow should be controlled to maintain a differential pressure cascade to prevent air from less clean areas (e.g. ISO Class 8 areas) from entering the cleaner areas (e.g. ISO Class 7 areas).
People are recognised as the biggest contributor of contamination in the cleanroom. Improperly gowned employees may shed microbial (e.g. staphylococcus epidermidis) and non-microbial (e.g. skin cells or hair) particles. People may transport particles when moving from room to room, as can materials (e.g. consumables, carts) that are not appropriately cleaned. Sinks, drains, standing water, or other water sources can also be sources of microbial contamination.
Chemical residues
Chemical residues from active ingredients or from drug products that may be hazardous (e.g. cytotoxic), sensitising (e.g. beta-lactams), or highly potent (e.g. hormones) may be deposited on work surfaces that are not properly cleaned or are not cleaned at an appropriate frequency.
Producing drugs without adequate controls to prevent these types of cross-contamination is an insanitary condition and could potentially lead to patient harm. The use of active ingredients or excipients with high levels of impurities (e.g. chemicals that are not intended for pharmaceutical use) may also cause patient harm.
Pests and other animals
It comes as no surprise that the presence of pests such as insects or rodents, the particles they shed, and their urine and fecal matter are examples of insanitary conditions. Compounding facilities should have robust pest control programmes designed to prevent pests from entering or nesting in or near drug production areas.
We have observed facilities whose staff brought in their pets from home. Companion animals should not be in compounding facilities for the same reasons that pests should not be present.
How to control contamination
1. Cleanroom design: Cleanrooms should be designed with personnel and material flow in mind. The critical area (ISO Class 5 area) where sterile drugs are handled should ideally be located in or protected by an ISO Class 7 cleanroom. This design, in conjunction with other controls, limits the introduction of microbial and non-microbial particles into the cleanrooms and critical areas such as the ISO Class 5 laminar flow hoods or ISO Class 5 biological safety cabinets. Doors or passthroughs that permit material flow directly between unclassified areas and the ISO Class 7 cleanroom where aseptic operations are taking place is an example of an insanitary condition.
2. Air flow: Air supplied to cleanrooms should be properly filtered. Facilities often achieve this goal using high efficiency particulate air (HEPA) filters. HEPA filters should be placed in the ceiling and air returns should be placed on the walls, low to the ground.
The airflow should sweep particles down and out of the cleanrooms. Loose ceiling tiles or non-ducted air returns may introduce particles into the cleanroom. Improper design can also cause turbulent airflow, which can introduce particles into the critical areas. Facilities should regulate the airflow to maintain a differential pressure cascade between areas of higher air quality and areas of lower air quality.
3. Cleaning and disinfection: All surfaces in the cleanrooms should be routinely cleaned and disinfected to remove microbial and non-microbial particles. The disinfectants and wipes used in the cleanrooms and critical areas (e.g., ISO Class 5 laminar flow hoods) should be sterile. For disinfectants to be effective, they must be applied for the required wet contact time (dwell time). Items should be disinfected before being introduced into the ISO Class 5 area or when moving from any area of lower cleanliness (e.g., ISO Class 8 room) to an area of higher cleanliness (e.g., ISO Class 7 room).
4. Environmental monitoring: Environmental monitoring includes monitoring viable microbial particles on surfaces (e.g., ISO Class 5 workbench), personnel (e.g., fingertip testing), and counting viable and non-viable particles (i.e., microbial and non-microbial particles) in the air.
Information from environmental monitoring helps to promptly identify potential routes of contamination and permits the implementation of corrective actions before more serious problems arise.
5. Personnel behaviour in cleanrooms: Operators preparing drugs that are intended to be sterile should be trained in aseptic technique and cleanroom behaviours, which include but are not limited to:
- Properly wear gowns and sterile gloves that are changed when necessary
- Disinfect gloves before entering the ISO Class 5 critical areas
- Move slowly and deliberately in the cleanroom to minimise disruption of the airflow that is intended to sweep particles out of the cleanroom
- Avoid blocking first air with items or with their bodies to ensure that aseptic manipulations performed in the ISO Class 5 critical area are only exposed to first air
- Avoid manually touching direct product contact surfaces to prevent contamination
Compounding facilities that prepare drugs are responsible for taking the necessary actions to protect patients and public health, including recognising insanitary conditions and taking steps to prevent and correct them.
Many serious patient illnesses and deaths associated with poor quality compounded drugs have occurred since the 2012 fungal meningitis outbreak. The FDA issues compounding risk alerts to inform health care professionals, compounders, and consumers about risks associated with compounded drugs, including information on adverse events, outbreaks or product quality issues.
The FDA has been diligently working to help compounding facilities enhance the quality of their compounding practices and comply with regulatory requirements enforced by the Agency. Part of our work involves the creation of FDA guidance documents, which outline the agency's thinking on a broad spectrum of topics. FDA created the Compounding Quality Center of Excellence to help improve the overall quality of compounded drugs, primarily those made at outsourcing facilities. Instructor-led and web-based trainings have been developed on a range of topics that can be found on our website.
We have observed facilities whose staff brought in their pets from home
The free online trainings are a good way for pharmacists, physicians, technicians, and others to learn more about cleanrooms, sterile drug processing and insanitary conditions, and much more. We also urge pharmacists and employees of compounding facilities to carefully review our final guidance on insanitary conditions.
If a compounding facility produces drugs under insanitary conditions, the facility and responsible individuals may be subject to regulatory actions. Compounding facilities should proactively work to protect patients from receiving poor quality compounded drugs. When there is a steadfast commitment to quality and vigilance that protects public health, everyone wins.
